Rotator cuff repair
Make an AppointmentAnatomy
Your shoulder has numerous muscles and tendons controlling movement and stability of the shoulder.
Among these are the tendons of the rotator cuff. The rotator cuff is composed of four tendons that blend together to help stabilize and move the shoulder.
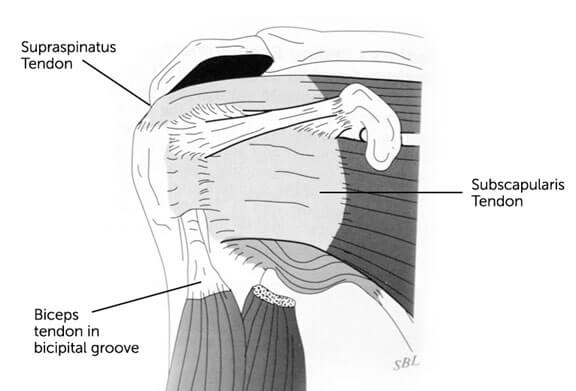
The rotator cuff is the collective term for a group of tendons, which includes the supraspinatus, infraspinatus, teres minor, biceps and subscapularis. (Fig. 1) These tendons pass under a bony-ligamentous arch.
Fig 1
What causes problems with the rotator cuff?
Problems can arise within the rotator cuff when it is:
• Irritated, bruised or frayed
• Weak, the bursa is swollen or the bony arch angles too far down
• Calcium deposits form within it
• Torn either partially or completely
Irritation, bruising or fraying of the tendons can occur with repetitive use of the arm e.g. When carrying heavy luggage or during sports like golfing and tennis. When the tendons are inflamed but not torn then it is called tendinitis. The pain is primarily from the inflamed tendons being rubbed by the bony ligamentous arch. This can also result in a bursitis, where the bursa above the tendons also becomes irritated and swollen which causes pain. The biceps tendon can also become frayed or unstable and may require treatment at the same time.
Tearing of the rotator cuff can occur when these tendons become irritated and swollen and eventually wear out or else they can occur as a result of a major force eg, direct injury. Most tears have some degree of preceding wear changes. Any accidents or injuries that might occur at work, sport or a fall may precipitate a tear of these weakened tendons.
Tears of the rotator cuff tendons occur with increasing frequency as the population gets older. It is unusual for a patient younger than 40 years to have a tear whereas up to 50% of patients over the age of 75 years have a tear in one or other rotator cuff tendon. A tear of the rotator cuff does not always have to be painful.
What are the symptoms?
The most common symptoms which cause a patient to seek medical advice are:
• Pain
• weakness and
• inability to raise the arm
How is a diagnosis made?
In determining the diagnosis it is most important to take a thorough history from the patient and also to examine them to assess their range of motion and ability to use and raise their arm. After this, one or more of the following tests may be ordered – a plain x-ray, ultrasound or MRI in order to assess the condition of the bones, tendons and ligaments.
How are these problems treated?
In patients who have an acute rupture of their rotator cuff after a fall, surgical management is generally indicated to restore function to the arm, however the majority of rotator cuff tears are degenerative in nature and occur over time. These ones rarely require surgery and are best managed with non-operative management.
Non-operative treatment includes:
• Physiotherapy (stretches/strengthening)
• Anti-inflammatory medication
• Activity modification
• Cortisone (steroid) injections
If this does not help in reducing the pain or if there is poor shoulder function then surgery maybe recommended. For those patients with a rotator cuff tear, a rotator cuff repair is performed.
How is the operation done?
Rotator Cuff Repair:
The purpose of the surgery is to reattach the torn tendon back to the bone.
Under a general anaesthetic, the arthroscope is firstly introduced into the shoulder joint and all pathology is identified. Any surgery that can be done through the arthroscope is done at that time. With small to medium sized tears and good quality tendon the repair can be done through the arthroscope through 3 or 4 separate small incisions. (Fig. 2)
Biceps tenodesis:
This operation involves re-anchoring the biceps in a better position to stop it slipping out of its groove or becoming irritated.
Fig. 2
Black lines are the patient’s bony anatomy landmarks. The solid red lines represent incisions for arthroscopy and arthroscopic rotator cuff repair. The dotted red line shows the mini open incision I use for larger rotator cuff tears and biceps tenodesis.

Fig 2
If however the tendon tear is large, I prefer to repair the tendon through a small incision 3 to 4 cm long at the side of the shoulder.
This is called a mini open repair and gives excellent exposure of the tendon. The outcome and rehabilitation of an arthroscopic repair or mini open repair are no different and the result of rotator cuff surgery really depends on the quality of the tendons at the time of the repair. The rotator cuff tear is then repaired by suturing it back to the bone using stitches and bone anchors.
All tears are different and a variable number of sutures and bone anchors can be used. An example is illustrated in Fig. 3. The operation involves coming into hospital for 1 night.
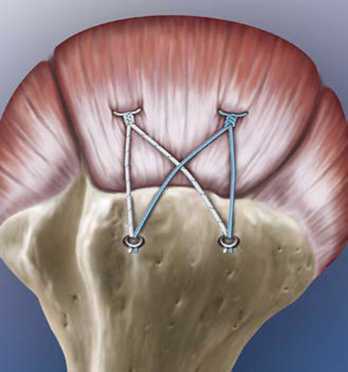
Fig 3
What happens after surgery?
You will be placed in a sling for 6 weeks to protect the repaired tendon. A physiotherapist will show you circular or pendular exercises, which you need to do for 6 weeks to prevent stiffness. Healing of the tendon is slow and it can take between 6 to 12 months to gain full recovery.
You MUST NOT raise your arm that has been operated on at all or lift anything heavier than the weight of a full coffee cup / can of drink with this arm for the first 6 weeks. Always put your sling on when you go out.
Complications related to the surgery can occur but are quite rare. A general anaesthetic is used and there are risks related to this. Some of the risks include infection, nerve and blood vessel damage. Occasionally the shoulder may develop some transient stiffness called capsulitis. This usually resolves itself however it delays the time taken till the shoulder recovers.
What happens on the day of the operation?
When the staff at the room’s book you in for surgery, they will advise you of when you must fast (stop eating and drinking) and present at the hospital. These times may change and you will be notified by either the hospital or the rooms a day or two before the surgery of any changes.
At the hospital, you will be seen by your anaesthetist who will ask questions about your health and talk to you about the anaesthetic he/she will give you.
What happens when I get back to the ward?
When you return to the ward you will have:
• a drip in your arm
• your arm in a sling
• regular pain relief
You will be able to drink and eat as soon as you are awake and alert. Your vital signs (blood pressure, pulse, temperature) will be checked overnight.
What happens during the rest of my stay in hospital?
You will be given regular pain-relieving tablets. It is important to have these regularly in order to keep your pain at a tolerable level to enable you to move about and exercise.
A physiotherapist will show you exercises to be done for the first 6 weeks and how to put on and take off your sling. You will be able to go home mid-morning the day after surgery.
I will see you 2 to 3 weeks after surgery to remove your dressings and check your wounds. I use dissolvable stitches, so I will not need to remove any stitches.
Frequently Asked Questions
Q: Does it hurt? What can I do to control the pain?
A: You will have pain but this should be relieved by the pain relief medication you are discharged from hospital with. Please let the hospital staff know of any allergies or sensitivities you have to any medication. You will need to take these regularly for the first week and then decrease them as the pain lessens.
In addition to medication, the following points may help you to get comfortable more quickly:
Ice. This may help to numb your shoulder for the first 48 hours though after this is may be of less benefit. Remember to always cover the icepack with a cloth so that it never makes direct contact with your skin.Come out of your sling. Often straightening your arm out and taking the pressure if the strap off your neck is a great way to ease discomfort.Avoid lying flat in bed at night. Arrange either 3 or 4 pillows into a “boomerang” shape behind you so that when you lie back, your shoulders are off the mattress and well supported by the pillows.Please advise us at the rooms if your pain is not relieved by taking the tablets regularly or if it suddenly becomes worse or severe.
Q: Do I need to redress the wound?
A: You should not need to change or remove the dressing that will be on your wound. These dressings are waterproof enabling you to shower and wash without worrying about wetting the wound. You may see some blood beneath the dressing but this will not cause any harm and can remain as is until you are seen about one week after your operation. If this dressing should come off do not worry, just replace it with another waterproof dressing.
Q: Can I shower at home and if so, how?
A: We do not recommend soaking in a bath until your wound has healed completely but showering is perfectly fine. Please take your sling off to shower. You may prefer to have some assistance with showering until you become more confident. As you are unable to raise your arm to wash under it, you should bend forward so that your arm gently swings forward enabling you to wash your armpit.
Q: I am having trouble sleeping. What do I do?
A: Many patients have told us that they find it difficult to get comfortable. Try setting up a “tri-pillow” or boomerang-shaped arrangement so that your back and shoulders are supported by pillows and also remember to take your pain relievers before going to bed.
Q: How often will I need to come back to see Dr Gohil after my operation?
A: You will see Dr Gohil when your stitches are removed and then further follow-up will be determined according to your rate of progress. You should expect to see him one week after the surgery, 5 weeks later, and at 3 and 6 months after surgery.
Q: When can I drive?
A: Driving a motor vehicle is usually not recommended for 6 weeks after the surgery, when the arm is comfortable and the vehicle can be safely controlled in an emergency. Driving with one arm in a sling is NOT recommended.
Q: When can I return to work?
A: Some employers will not allow a worker to return wearing a sling and therefore in those circumstances you should expect to be off work for 6 weeks. Patients needing to go back to light manual tasks would need to allow an average 4-6 months recovery. They would not be able to lift overhead or do repetitive actions above shoulder level for about 6-12 months
Q: When can I play sport?
A: You cannot return to contact sports until your shoulder has been reassessed 6 months after surgery, and then only if you have excellent strength and coordinated control of your shoulder.
Q: Will I need physiotherapy?
A: Yes, though a formal physiotherapy programme does not usually commence until you come out of your sling completely 6 weeks post op. For the first 6 weeks, you are the best physiotherapist and at your first visit after surgery, you will be shown some simple exercises to do at home. Even though your arm is to remain in a sling for the next few weeks, you must remove the sling 3 times a day for passive motion excercises.
Using the arm before the healing is complete can cause the repair to fail. On the other hand, immobilising the shoulder for a long period to protect the repair can cause shoulder stiffness. For these reasons careful postoperative rehabilitation is an essential part of your surgery. There are two aspects of the rehabilitation programme; preventing unwanted scar formation and protecting your repair.
Q: How successful is this surgery?
A: The secret to successful rotator cuff surgery is for you to be patient in order to achieve the desired result
The tendon generally takes 3 months to reattach to the bone and then it takes you another 3 months or longer for you to achieve a functional range of motion and strength.
I always tell patients that the result of surgery depends on the patient’s tendon quality not my surgery. If you have a thin and poor quality tendon then the result will not nearly be as good as someone that has a thick and robust tendon that can easily be reattached to its anatomical position.
Patients also have to understand that pain can continue over the first 3 months and then it generally settles with time.
Be patient as there are no shortcuts in this surgical procedure. It will take 6 to 12 months to get over the procedure and the majority of patients are glad they have had the operation.
SHOULDER ARTHROSCOPY AND ROTATOR CUFF REPAIR
You have been booked for a Shoulder Arthroscopy and Rotator Cuff Repair and Mr. Gohil has given both verbal and written information. Please read these and if you have any questions contact us.
This usually requires an overnight stay so you will be admitted on the day of surgery, and be going home the following morning after surgery.
Tests
You have been given forms for investigation. These need to be completed at least 2 days before your surgery. If you are having X-rays, please bring these and any relevant tests with you on the day of surgery (e.g. Ultrasound / MRI). The results of your blood tests and ECG (if requested) will be sent to us.
Anaesthetist
Your anaesthetist will be Dr. Harper, Dr.Crossley, Dr. White or Dr. Thompson, who will contact you by telephone before the day of surgery to explain about the anaesthetic. They will see you on the day of surgery in the hospital.
Admission
You will be contacted by admissions a day prior to surgery to confirm the surgery and time of admission. You need to be fasting (no food) for 6 hours prior to surgery and nothing to drink for 2 hours prior.
What to bring
- Your MRI and X-rays and other scans ordered (e.g. Ultrasound / CT)
- All your medication
- Change of clothes with comfortable non-slip flat shoes
- Please arrange for someone to pick you up from the hospital and you may need some help at home for a couple of days.
After the surgery
You will be admitted to the ward after your surgery. A physiotherapist will review you on the ward and if necessary arrange outpatient physio.
You will be in a sling for 6 weeks. There will be a pressure dressing on the shoulder and this needs to remain on for 72 hours. The waterproof dressings can then be changed to a clean waterproof dressing, then changed every third day if required. The incisions should be covered for 2 weeks until seen in the clinic.
What to expect following the procedure
Swelling and some bruising are common and can affect the arm all the way down to the elbow but will resolve. If there is increasing swelling or wound discharge and redness go see your doctor or give the rooms a call.
You will be given pain relief on discharge, and you may need to get a further prescription.
Bleeding-there may be a little blood on the dressing. This should settle down once you change the dressing.
You will be given some pendulum exercises by the physiotherapist for the first 6 weeks. After this you will be able to move your arm actively and use of the sling is for comfort only. You should not need a sling after 6 to 8 weeks.
Follow up
You will be contacted with a follow up appointment to review your progress, and at this appointment Mr. Gohil will advise you about driving and returning to work.
Contacts
Rooms on 0893121135
Further information is available on our website: www.orthopaedicswa.com.au
Make an appointment with Mr Satyen Gohil.
Please get in touch with us by completing the form here or alternatively you can contact us by fax or phone at the numbers below. We will endeavour to get back to you as soon as possible.
