Matrix Induced Autologous Chondrocyte Implantation (MACI)
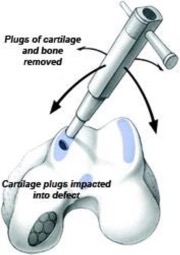
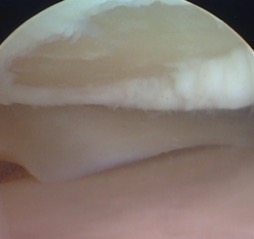
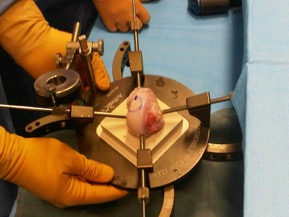
MACI is a two-step procedure in which new cartilage cells are grown and then implanted in the cartilage defect.First, healthy cartilage tissue is removed from a non-weightbearing area of the bone. This step is done as an arthroscopic procedure. The tissue which contains healthy cartilage cells, or chondrocytes, is then sent to the laboratory. The cells are cultured on a collagen matrix (a biologic scaffold) and increase in number over a period of 6 weeks.
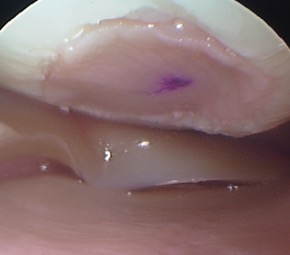
An open surgical procedure, or arthrotomy, is then done to implant the newly grown cells onto another collagen matrix, which is secured within the defect using fibrin glue (a biologic adhesive). MACI is most useful for younger patients who have single defects larger than 2 cm in diameter.
Advantages of MACI:
- It provides more durable hyaline cartilage.
- By using the patient's own cells, there is no danger of a patient rejecting the tissue.
Potential disadvantages of MACI:
- It is a two-stage procedure that takes several weeks to complete.
- It requires an open incision.
Matrix Induced Autologous Chondrocyte Implantation (MACI)
MACI is a two-step procedure in which new cartilage cells are grown and then implanted in the cartilage defect.
First, healthy cartilage tissue is removed from a non-weightbearing area of the bone. This step is done as an arthroscopic procedure. The tissue which contains healthy cartilage cells, or chondrocytes, is then sent to the laboratory. The cells are cultured on a collagen matrix (a biologic scaffold) and increase in number over a period of 6 weeks.
An open surgical procedure, or arthrotomy, is then done to implant the newly grown cells onto another collagen matrix, which is secured within the defect using fibrin glue (a biologic adhesive).
MACI is most useful for younger patients who have single defects larger than 2 cm in diameter.
Advantages of MACI:
• It provides more durable hyaline cartilage.
• By using the patient's own cells, there is no danger of a patient rejecting the tissue.
Potential disadvantages of MACI:
• It is a two-stage procedure that takes several weeks to complete.
• It requires an open incision.