Meniscal tears
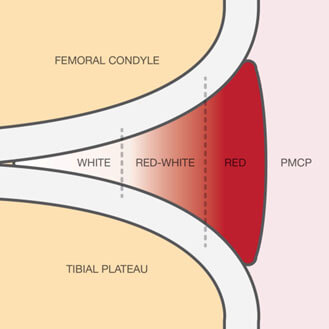
Make an AppointmentThe meniscus is a fibrocartilaginous structure made of predominantly Type 1 collagen. (Fig. 1) It optimises force transmission and acts as a shock absorber in the knee, ultimately protecting the underlying cartilage. The medial meniscus also acts as a secondary stabiliser of anterior knee translation. The outer 1/3 of the meniscus has a blood supply and is termed the ‘red zone’. (Fig. 2) Tears that involve the outer 1/3 have the most favourable prognosis when it comes to meniscal repair.
Fig. 1 – Superior view of a tibia with anatomy of the menisci
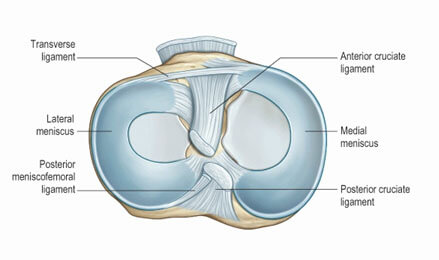
Fig. 2 - Front view of a meniscus sectioned showing the different zones. Only the outer 1/3 or ‘red zone’ has a blood supply
What types of meniscal tears are there?
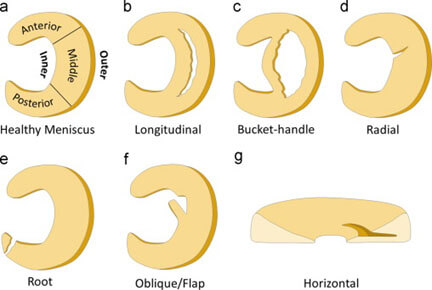
Tears are either traumatic or degenerative. (Fig. 3)
The management of traumatic tears in the setting of ligamentous injury of the knee in young patients is fairly clear cut. Meniscal repair or preservation in combination with a stable knee lead to less long-term degeneration in the knee. So, in the setting of an ACL injury, we make every attempt to perform an ACL reconstruction and meniscal repair if possible. The management of the degenerative meniscal tear in the setting of arthritis remains controversial and there is a body of evidence that arthroscopic debridement compared to non-operative treatment has similar outcomes.
Fig. 3 - Types of meniscal tear
What are the clinical signs of a meniscal tear?
Usually a small effusion in an acute tear.
Joint line tenderness.
Positive Mcmurray test.
Knee hyperflexion usually reproduces patient’s symptoms.
What are the indications for meniscal repair?
Usually traumatic meniscal tears in young active patients. Meniscus preservation gives longer term cartilage protection and every attempt is made to try and prevent later knee degeneration.
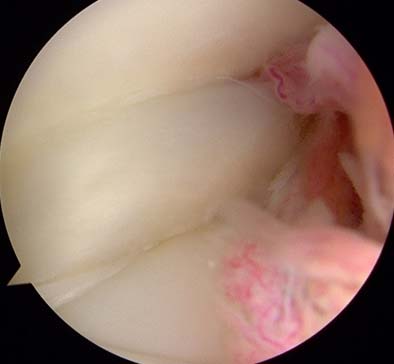
Locked knee due to a bucket handle tear of the meniscus is considered an Orthopaedic emergency. (Fig’s 4 and 5)
Fig. 4 a and b – Sagittal MRI showing a bucket handle tear of the lateral meniscus. The flipped meniscus is shown arrowed in the anterior knee and in the second slice a ‘double pcl’ is seen, with meniscal tissue in the intercondylar notch.


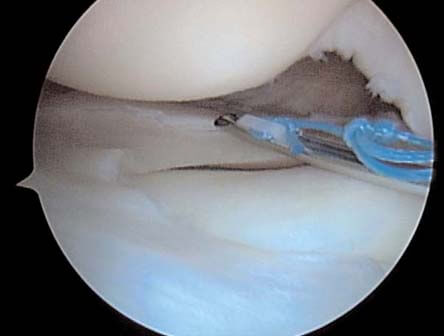
Fig. 5 a and b – Arthroscopic view of the same knee showing the bucket handle tear flipped anteriorly. This has then been reduced and fixed with an all inside suture technique.

Vertical longitudinal tears in the peripheral zones of the meniscus are more likely to heal due to proximity to the meniscal blood supply. (Fig. 6)
Fig. 6 a and b – Peripheral longitudinal lateral meniscal tear in the red/white zone being repaired with an all inside technique.

Combined ACL injury with meniscal tears. Meniscal repair protects the knee from further instability and degeneration in combination with ACL reconstruction.
Complete radial tears reaching the periphery of the meniscus should be repaired to restore ring continuity.
Meniscal root tears. Lateral root tears are usually traumatic and associated with ACL tears. Trans-osseous repair of the root maintains hoop stresses in the meniscus and prevents extrusion, thereby offering some protection from cartilage degeneration. (Fig. 7)
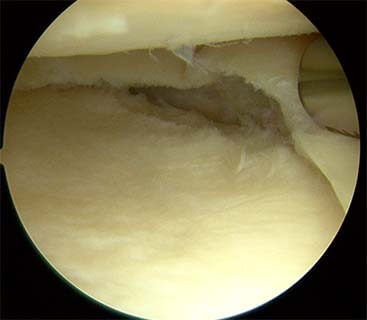
Fig. 7 a and b – Arthroscopic photos of a posterior root lateral meniscal tear with meniscal extrusion in the setting of ACL rupture. The root is not attached posteriorly. First photo shows a trans tibial tunnel used for passing the sutures already placed in the root. Second photo shows the completed repair.


Degenerative meniscal tear management in the middle aged to elderly is controversial. In the first instance, simple analgesics and NSAIDS can be tried, followed by a steroid injection at least 6 weeks after onset of symptoms. Weight bearing AP radiographs and patella skyline views should be routine to exclude significant osteoarthritis. If symptoms don’t settle after 2-3 months and the patient still complains of mechanical symptoms such as clicking, catching or locking then a referral to a specialist and MRI can be performed for consideration of an arthroscopic debridement. (Fig. 8)
Fig. 8 a, b and c – Degenerative flap tears in the setting of mild arthritis. Note the irregular chondral surfaces. Last photo shows the resected meniscus. This configuration does well following arthroscopic debridement.


Medial root tears often degenerative. Attempt repair if less than grade 1 or 2 chondromalacia. Prognosis generally poor. If grade 3/4 chondromalacia then worth trying intra-articular steroid injection and watching for 6 weeks. Can consider an arthroscopic debridement if symptomatic after that. Can ultimately lead to total knee replacement.
Rehabilitation after meniscal repair
Patients are usually allowed to full weight bear with a hinged knee brace and allowed 0-90-degree range of motion for 6 weeks. Flexion past 90 degrees increases stresses at the repair site and can lead to failure.
If a root repair is performed, patients weight bear in extension for 2 weeks followed by 4 weeks at 0-90 degrees of flexion.
Following meniscectomy, early weight bearing and full movement is encouraged usually without crutches.
Summary
With the right indications, meniscal preservation rather than resection should be considered. This is usually in the setting of traumatic meniscal tears in young individuals.
In degenerative tears a trial of conservative treatment is indicated in the first instance, with surgery reserved for those who have not responded to conservative treatment in the setting of mechanical symptoms.
There is no indication for meniscectomy in the setting of advanced OA. More than likely this will lead to some form of arthroplasty.
Frequently Asked Questions
How to make an appointment?
Please contact my secretary Silvana on 0428 585 601 or (08) 9312 1135
Fax: (08) 6161 1664
Email: silvana@orthopaedicswa.com.au
Do I need a Doctor’s referral to see Mr. Gohil?
Yes, a written referral from a registered practitioner in Australia is required.
A referral from a GP lasts 12 months, and a referral from another specialist lasts 3 months.
The backdating of referrals is illegal.
Where else does Mr. Gohil work and operate?
Mount Hospital
Fremantle Hospital
Fiona Stanley Hospital
Patient info
Mr. Satyen Gohil is a no gap provider for all health funds (provided your health fund covers the procedure), meaning that for the surgery, there no extra costs charged to the patient for the surgery or anaesthetic above that which is covered by the health funds.
Initial consultation cost is $200 Follow up appointments are $100 There are no further costs for post-operative visits for the first 6 weeks, after which time the cost of each visit is $100. Workers compensation and MVIT consultation fees will be sent direct to the insurer. However, if the claim number is not provided you will be responsible for settling the account on the day.
Blood tests
There is an out of pocket charge for blood tests.
Anaesthetist
Your anaesthetist will be Dr. Harper, Dr.Crossley, Dr. White or Dr. Thompson, who will contact you by telephone before the day of surgery to explain about the anaesthetic. They will see you on the day of surgery in the hospital.
Radiology
X-rays as an inpatient are covered, but outpatient X-rays and CTs within the hospital have an out of pocket cost.
MRI costs vary considerably depending on where they are done. Please ask for more details.
www.skg.com.au
Cardiology
For ECG (heart tracings) I use WA cardiology as appointments are not needed. There is a charge above the Medicare rebate.
www.wacardiology.com.au
Medical reports and insurance forms
Are charged at a rate representing the time taken to complete the forms.
Full payment at the appointment time is appreciated. Cash or credit cards are acceptable means of payment. For bank and personal cheque please make prior arrangements with the reception.
Useful links
Medicare Australia
http://www.medicareaustralia.gov.au/
St John of God Murdoch Hospital
http://www.sjog.org.au/hospitals/murdoch.aspx
Department of Veteran Affairs
http://www.dva.gov.au/Pages/home.aspx
Make an appointment with Mr Satyen Gohil.
Please get in touch with us by completing the form here or alternatively you can contact us by fax or phone at the numbers below. We will endeavour to get back to you as soon as possible.
