Total Knee Replacement
Make an AppointmentTotal knee replacement (TKR) has become one of the commonest surgeries that we perform, and has been very successful in alleviating the pain and dysfunction associated with arthritis.
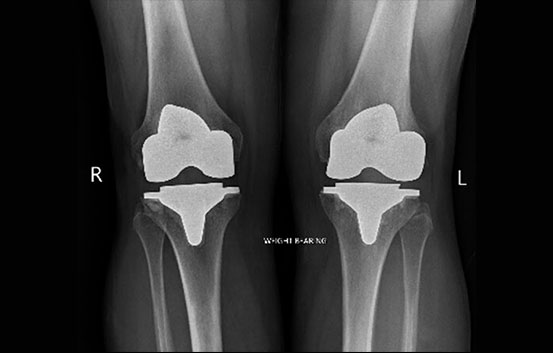
The TKR is made up of three components (Fig's 1 and 2); the femoral component covers the end of the femur (thigh bone), the tibial component sits on top of the shin bone, and the patella resurfaces the back of the knee cap. Between the femoral and tibial components is the bearing, which is made of a very hard plastic. Recent technological advances in bearing materials have improved this material, reducing wear, which should increase the longevity of the knee replacement. The knee can be fixed to the patients bone by cement, or can come in direct contact to the bone and allow a living biological bond to form between the implants and the bone.

Indications
Cause of arthritis of the knee:
Unlike arthritis in the hip, the majority of knee arthritis is caused by injury to the structures within the knee, or wearing out of the cartilage. There are other secondary causes such as infection, malalignment, trauma, dysplasia, inflammatory disease, avascular necrosis, and knee disease often runs in families suggesting an inherited problem.
Total knee replacement is the last resort for most knee conditions, and often patients will have had other more conservative procedures such as trimming of the cartilage, ligament surgery etc. In some people, where the knee arthritis is isolated to one part, they can be treated by either realigning the leg (osteotomy), or replacing only the arthritis part (unicompartmental knee) or patello femoral replacement.
The decision to undergo total knee replacement always remains with the patient. The surgeon makes sure of the diagnosis and advises the patient of the implications and possible complications. Pain and loss of function are the most important indications for joint replacement surgery.
Pain
Different people have different pain thresholds and also respond to painful diseases differently. We often try and quantify pain by the number of painkilling tablets or analgesics patients take each day, what the pain stops the patient from doing, and if their sleep is affected. If this pain cannot be controlled by other measures surgery is indicated.
Loss of function
Once again there is no absolute guideline as this is a very individual interpretation based on the patient’s own expectations of mobility and function.
Both of these factors affect the quality of life of the patient, at home and at work. When the quality of life is affected to an unacceptable level by the disease, and not controlled by other not surgical measures, then surgery should be considered.
Implant survival
Joint replacement was previously reserved for elderly patients because we know that over 80% of implants will survive 20 years, but may survive less in the more active and demanding younger patients. There is no doubt that joint replacement can make an enormous positive difference in quality of life in younger patients, and should not be denied to them. However, the likelihood of further re-do surgery is inevitable, and this presents potential future problems for these patients.
Contraindications to TKR
There are very few contraindications to TKR. However, some patients may be at very high risk of complications, and some may need special facilities such as ICU. The presence of active infection is a contraindication to primary knee replacement.
Results
Knee replacements are very reliable at reducing the pain of arthritis, and providing a stable knee for daily activity. However, they rarely feel like a natural knee, and bending is usually limited to about 110-120 degrees. I do not recommend that you run on any knee replacement, and sport is limited. Kneeling is not usually improved after TKR.
Knee replacement surgery is much more painful than that for hips, and recovery takes much longer. This is because knee function is so dependent on the recovery of the muscles and soft tissues. I expect pain and function to continue to improve for nine months after surgery.
Possible Complications Include
Infection <1%
Organisms are usually introduced onto the prostheses at the time of surgery from the patients skin, or just after surgery from wound problems. Occasionally infection can spread from a distant site to a well functioning prosthesis. Once established, infection is hard to eradicate without removal of the prostheses. Extensive surgery is usually required usually in 2 stages, and results can be poor.
Thrombosis/Pulmonary embolus 1%
Thrombosis in the deep veins of the leg (DVT) are common after knee surgery, however rarely do these cause any problem and they need no specific treatment. About 1% of patients will have a DVT that requires treatment either because of calf pain, or when the thrombosis has spread into the thigh. About 1 in 1000 patients will have a thrombosis that will travel up into the lung (PE) where it can cause serious problems including death. All patients are assessed for risk preoperatively. Routine preventative management is by minimizing operative time, keeping the patient hydrated, regional anaesthetic (if possible), foot/calf pumps to circulate the blood, and early mobilization. I do not believe that heparin significantly reduces the risk of thrombosis, and definitely causes wound problems. I treat high-risk patients with warfarin for 6 weeks after surgery.
Anaesthetic complications <5%
Complications may result from the anaesthetic and stress of the surgery. Patients are carefully assessed preoperatively in order to try and minimize these risks, but clearly patients with some medical problems such as diabetes and heart conditions will be at higher risk. Risk can be further minimized by optimizing preoperative health, such as stopping smoking, reducing excessive weight, balanced diet etc.
Bleeding
About 5% of my patients require transfusion after this operation.
Death (very rare).
Stiffness (<5%)
Stiffness after knee replacement is strongly associated with stiffness before the operation. Careful examination and investigation is required as there are many causes of this that can be hard to define. Secondary causes include: infection, component malposition, allergy to metal, muscular problems, and hip disease. Occasionally it is amenable to a manipulation under anaesthesia, but often requires specialist assessment and revision surgery.
Continued pain 10-20%
Unfortunately, a significant number of patients continue to experience pain after TKR. Again, this needs careful evaluation by a specialist to look for a treatable cause.
Anterior numbness
All approaches to the knee for this surgery require sacrifice of a small nerve at the front of the knee that supplies the feeling to the skin on the outside of the knee. This area will be numb after the surgery, and as nerves grow back into the area, patients may feel pins and needles, or sometimes pain. This can be dealt with by massaging the area, which just helps “re-educate” the nerves. This process usually takes about three months, after which time an area of numbness may remain.
Loosening
Modern implants may become loose after many years of use. This is often associated with wear, or mal alignment.
Wear
The moving parts of all prostheses wear, causing bone loss and loosening of prostheses. Modern materials are harder wearing so that wear is becoming less of a problem.
Fracture <1%.
This is rare, but more common in complex operations, deformity or revision operations. Most can be dealt with during surgery, but occasionally they are only picked up after surgery and may require intervention.
Vascular injuries < 1 in 1000.
Penetration or incision of an artery or vein.
Nerve injuries < 1 in 1000.
Activity after TKR
Walking and normal daily activity is encouraged after TKR, but impact sport is probably damaging. If you are to have any invasive procedures after a TKR such as dental work, bowel surgery etc. please inform your treating professional that you have a joint replacement, as you may need to be given antibiotics to protect the prosthesis from infection. The highest risk for this is within the first three months.
I provide a good range of treatment for arthritic disease of the knee including, arthroscopic treatments, meniscal surgery, osteotomy, unicompartmental knee replacements, and total knee replacement.
X rays showing before and after total knee replacements.

Frequently Asked Questions
How to make an appointment?
Please contact my secretary Silvana on 0428 585 601 or (08) 9312 1135
Fax: (08) 6161 1664
Email: silvana@orthopaedicswa.com.au
Do I need a Doctor’s referral to see Mr. Gohil?
Yes, a written referral from a registered practitioner in Australia is required.
A referral from a GP lasts 12 months, and a referral from another specialist lasts 3 months.
The backdating of referrals is illegal.
Where else does Mr. Gohil work and operate?
Mount Hospital
Fremantle Hospital
Fiona Stanley Hospital
Patient info
Mr. Satyen Gohil is a no gap provider for all health funds (provided your health fund covers the procedure), meaning that for the surgery, there no extra costs charged to the patient for the surgery or anaesthetic above that which is covered by the health funds.
Initial consultation cost is $200 Follow up appointments are $100 There are no further costs for post-operative visits for the first 6 weeks, after which time the cost of each visit is $100. Workers compensation and MVIT consultation fees will be sent direct to the insurer. However, if the claim number is not provided you will be responsible for settling the account on the day.
Blood tests
There is an out of pocket charge for blood tests.
Anaesthetist
Your anaesthetist will be Dr. Harper, Dr.Crossley, Dr. White or Dr. Thompson, who will contact you by telephone before the day of surgery to explain about the anaesthetic. They will see you on the day of surgery in the hospital.
Radiology
X-rays as an inpatient are covered, but outpatient X-rays and CTs within the hospital have an out of pocket cost.
MRI costs vary considerably depending on where they are done. Please ask for more details.
www.skg.com.au
Cardiology
For ECG (heart tracings) I use WA cardiology as appointments are not needed. There is a charge above the Medicare rebate.
www.wacardiology.com.au
Medical reports and insurance forms
Are charged at a rate representing the time taken to complete the forms.
Full payment at the appointment time is appreciated. Cash or credit cards are acceptable means of payment. For bank and personal cheque please make prior arrangements with the reception.
Useful links
Medicare Australia
http://www.medicareaustralia.gov.au/
St John of God Murdoch Hospital
http://www.sjog.org.au/hospitals/murdoch.aspx
Department of Veteran Affairs
http://www.dva.gov.au/Pages/home.aspx
Make an appointment with Mr Satyen Gohil.
Please get in touch with us by completing the form here or alternatively you can contact us by fax or phone at the numbers below. We will endeavour to get back to you as soon as possible.
